Many people are ashamed of touching upon such a delicate topic as sex organs. Nevertheless, all of us should know the anatomy of a human body, and sex organs are not an exception. Knowing our body helps to avoid different health problems.
Our today’s article is dedicated to the prostate, prostate diseases and methods of treatment of prostate cancer and BPH. The article is based on questions that you have sent to our email.
What is the function of the prostate?
The prostate gland secretes the seminal fluid and propels it into the urethra during ejaculation
What are the approximate size and weight of the prostate gland?
Normally, the size of the prostate is about 3 cm, and its weight is about 20 grams.
Why does the prostate become enlarged with age? When does it happen?
Prostate enlargement is a natural process, the same as, for example, graying. The prostate begins to grow when а man reaches 45 years. It is strange enough to see a man over 45 that doesn’t have an enlarged prostate. However, there is no scientific evidence why it is happening. On average, 80% of men have an enlarged prostate.
Where is the prostate located?
The prostate gland surrounds the urethra and is located between the bladder and the rectum.
What are the most common prostate diseases?
The prostate changes with age: it grows and becomes less elastic. When the prostate loses its elasticity, men deal with benign prostatic hyperplasia (BHP). As seen from the abbreviation, BHP is a benign tumor that develops in the prostate gland and does not grow beyond it. When the prostate increases, it puts pressure on the urethra and makes it harder for urine to pass through the urethra while urinating.
Inflammation of the prostate gland is called prostatitis.
Another disease is prostate cancer. In France, about 55000 new cases of prostate cancer are diagnosed annually. This type of oncology is considered the most common among men.

I am 56 years old, I have a frequent urge to urinate. Sometimes this urge is false, and I have urinary retention. The cause is BPH. Doctors say I need surgical intervention. What are the methods of the treatment of prostate enlargement? I do not want surgical intervention to affect my life and cause sexual dysfunction.
The most common treatment of BPH is laser therapy. However, this technique is becoming out of date and is becoming replaced by a prostate lift. In France, the prostate lift has been widely used since January 2017. This kind of procedure does not affect sexual potency. The prostate lift does not imply ablation, that is, the prostate gland remains in its place. What are prostate lift procedure steps? A special probe is inserted into the patient through the urethra; then the prostate gland is “tied up”, which causes urine output. Then the prostate is clipped on both sides with special implants that serve as a kind of corset and support the prostate. The prostate no longer compresses the urethra and does not interfere with normal urination.
The surgery is minimally invasive, it is performed mainly under local anesthesia. The patient does not feel any pain during the procedure. The surgery usually lasts 15-30 minutes. After the prostate lift, it takes some time for the implants to become overgrown with fibrous tissue.
The patient may experience some discomfort during urination for the first few days after the prostate lift.
This technique is quite new, accordingly, its effectiveness in the long term is not clear enough, but it is safe to say that prostate lift does not do any harm to the patient since the implants can be removed at any time.
There are a large number of biologically active additives (BAA) and drugs that allegedly treat prostate adenoma. However, it is scientifically proven that they are not effective, and the only way to get rid of this disease is to resort to surgical intervention.
I have prostate cancer. The doctor ordered a radical prostatectomy. They say that any method of surgery (open, laparoscopic or robotic) influences sex life. Is it really so?
Indeed, the removal of the prostate affects the patient's sex life, regardless of the method of surgery
Currently, open surgical techniques are rarely used, since they have several disadvantages: risks of infection, the presence of scars, long recovery. In France, open surgery has not been practiced for a long time, in 80-90% of cases, robotic prostatectomy with the da Vinci robot of different generations or laparoscopy are performed.
A total (radical) prostatectomy is rarely prescribed in France thanks to the development of robotic surgery, which allows to remove of only a tumor and maintain the prostate gland and all its functions. The higher the generation of the robot is the more pinpoint surgeries it may conduct. Robotic surgery minimizes the risk of infection, implies rapid postoperative recovery, and leaves no scars.
Ejaculation is impossible after total prostatectomy, but this does not imply erectile dysfunction. Many men can experience orgasm without erupting semen (dry orgasm).
After removal of the prostate gland, men often need a special penis simulator that helps to restore an erection. The simulator is a pump that promotes blood flow to the organ. There are other aids, such as creams and injections. Injections are given with very fine needles, so there is no discomfort during the procedure. The cream is applied to the external urethral orifice, after which the cream melts and is absorbed into the penis. Remember! Creams and injections will not help if there is no sexual desire!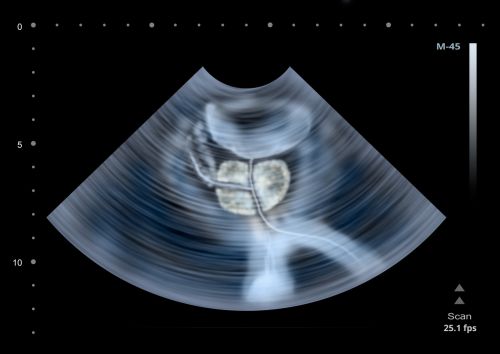
My father and grandfather had prostate cancer. Does this mean that I will have prostate cancer?
The genetic predisposition increases the risk of cancer, however, does not guarantee cancer. The genetic factor is just one of a number of factors that influence the onset of oncology. To prevent prostate cancer one should try to minimize the influence of harmful factors. It is necessary to get rid of bad habits, go in for sports, have regular sex, eat healthy ... You should also undergo a regular medical examination. Currently, Prostate-Specific Antigen (PSA) test is quite popular. An elevated PSA indicates prostate problems, not necessarily prostate cancer. Scientists conducted a study, during which 70,000 men had been taking a PSA test for 10 years, but the cancer mortality rate had not diminished. Some scientists say these tests are ineffective in preventing prostate cancer, while others say that ten years is not enough to test the effectiveness of PSA tests. French doctors contend that a PSA test should be regularly taken. When a PSA level is increased, you should see the doctor for a further examination or treatment.
If there are cases of prostate cancer among family members, you should regularly examine the prostate gland not from the age of 50, as recommended, but from 45 years.
Some urologists say that frequent ejaculation helps to prevent prostate cancer, is it true? If yes, how to explain it scientifically?
Indeed. There is a correlation between the number of ejaculations and the onset of prostate cancer. Those who erupt sperm more than 20 times a month, reduce the prostate cancer risk by 50%. There is no upper age limit when ejaculation is not beneficial. It is explained by the fact that there are two substances in the semen: spermine and spermidine, which are considered oncogenic, that is, they may transform healthy cells into malignant. Accordingly, these substances of semen should not be in contact with the prostate gland for a long time. Men should as often as possible propel the seminal fluid out to reduce its contact with the prostate. Coitus and masturbation may be considered preventive measures that help to reduce prostate cancer risk.
What is the difference between prostate cancer and BHP?
Prostate cancer has no symptoms at its initial stages, therefore, to diagnose it, it is necessary to take not only a PSA test but also a rectal examination of the prostate gland. After the rectal exam, the doctor may assign some other medical tests.
BHP (prostate enlargement) is a benign tumor that does not spread beyond the prostate gland. Prostate enlargement can cause sexual and urinary disorders.
Prostate cancer is a malignant tumor that can grow outside the prostate gland, metastasize to other organs and lead to death.
BHP can be distinguished from prostate cancer only by a urologist after rectal examination and laboratory tests.
Is high-intensity focused ultrasound (HIFU) used for treating prostate cancer?
This technique has been used for treating prostate cancer for many years. However, this type of treatment is not suitable for everyone. If the tumor is large enough and it touches the rectum, then ultrasound may burn the rectum. HIFU is used for treating tumors of a certain size located in a certain place.
The procedure of HIFU is performed under general anesthesia. The patient lies in a lateral position on a couch, while a special probe is inserted into the rectum to determine the exact location of the tumor. The program remembers this location, and then the tumor is processed by ultrasound waves. Ultrasound causes a rise in temperature (up to 100 - 180 degrees) and kills malignant cells. HIFU technique is robotic, however, the doctor watches the process in real-time through a special monitor. Sites having been treated with ultrasound are highlighted. High-intensity focused ultrasound procedure lasts for about 2 hours. In 2 days, the patient may be discharged from the hospital.
The advantages of HIFU: the absence of radioactive radiation; absence of pain; no side effects, the possibility of repeating the procedure in case of relapse.
What is prostate brachytherapy?
Prostate brachytherapy is a form of radiation therapy that is used for prostate cancer treatment. It is used at the initial stages of the disease when there is no need for surgical intervention. Brachytherapy is performed under general anesthesia. The patient lies in a lithotomy position and small implants with radioactive iodine-125 are implanted into his prostate gland close to the cancer cells. These applicators are equally implanted through a special metal grid. This procedure is carried out exclusively by a radiotherapist, while the radiotherapeutic technologist controls the process of implantation through the monitor, where the prostate, its shape, size, and location are clearly visualized.
The patient is discharged in 2 days after the procedure.
Implants remain radioactive for 6-8 months, and then they lose their radioactivity.







