Radiotherapy uses high-energy rays, such as x-rays to treat cancer. It destroys cancer cells in the area where it is given.
Some normal cells in the area can also be damaged by radiotherapy. This can cause side effects. These normal cells are usually able to repair themselves, but cancer cells cannot. As the normal cells recover, the side effects usually get better, and transitory.
Radiotherapy is always carefully planned by a team of experts (radiation oncologist and radiation physicist).
Radiotherapy treatment is continuing to become even more accurate. This allows your team to treat cancer more effectively while doing as little harm as possible to normal cells. The treatment is given 5 days a week, once per day, for 10 to 20 min. The treatment time depends on the number of sessions (5 to 35 sessions) decided according to the type of tumor, nodes or metastases, and the size of the lesions.
Why Radiotherapy?
Many people have radiotherapy as part of their cancer treatment. Radiotherapy is given for different reasons.
1. Radiotherapy to cure the cancer
This is when radiotherapy is given to try to destroy a tumor and cure cancer. You may have radiotherapy on its own or sometimes with chemotherapy (chemoradiation).
Radiotherapy can be given after surgery for some types of cancer, to lower the risk of cancer coming back (recurrence). This is called adjuvant (after=surgery) radiotherapy.
Sometimes radiotherapy is given before surgery to shrink cancer and make it easier to remove (neoadjuvant = before surgery).
2. Radiotherapy to treat symptoms such as PAIN
This is when radiotherapy is given to shrink cancer and help with symptoms such as pain or coughing. Doctors may suggest this treatment to help control cancer for longer when curing the cancer is not possible.
Ways of giving radiotherapy
- External beam radiotherapy is given from outside the body (externally) by a radiotherapy accelerator.
Radiotherapy treatment is planned carefully for each person. This means that even if you know someone with the same type of cancer as you, their radiotherapy treatment may be different. There are different types of external beam radiotherapy including that we use in our center:
- conformal – shape the radiotherapy beams to fit the treatment area
- intensity-modulated radiotherapy treatment (IMRT) – shapes the radiotherapy beams and gives different doses to different parts of the treatment area
- volumetric-modulated arc therapy (ARC) – the machine moves around you during treatment
- image-guided radiotherapy (IGRT) – uses images taken before treatment to check the position of the treatment area
- 4D – takes images during treatment to adjust for movement such as breathing
- stereotactic radiotherapy (SBRT or SABR) –Stereotactic ablative radiotherapy (SABR) is a way of giving radiotherapy. It is used to precisely target certain cancers. It is only suitable for some people, usually those with smaller cancers.
SABR uses small, thin beams of radiation directed from different angles that meet at the tumor. This means the tumor gets a high dose of radiation, while the surrounding healthy tissues get a low dose. This lowers the risk of damaging the healthy normal cells surrounding the tumour.
The treatment itself is painless. You may have between 1 and 8 sessions of treatment. Side effects of treatment may include tiredness, skin reactions, soreness, swelling.
Side effects may appear during treatment or just after your treatment finishes. They usually go away within a few weeks.
Stereotactic radiotherapy (SRT) is a type of radiotherapy used to treat some brain tumours. It is sometimes called Gamma Knife™ or CyberKnife™.
SRT uses many small beams of radiation that cross at the tumour. The tumor receives a high dose of radiation. Nearby areas are only affected by low doses.
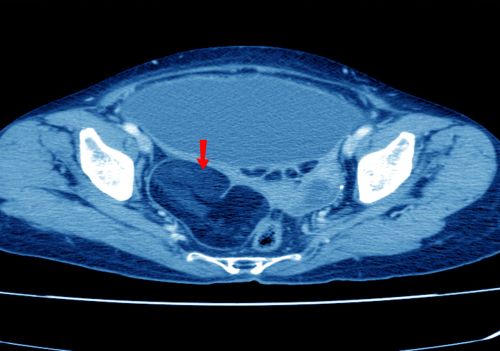
Your treatment is planned using a brain CT scan (computerized tomography scan) or an MRI scan (magnetic resonance imaging scan). You may need a mask or head frame made. This helps to keep you in a position during treatment. SRT is painless. Your radiotherapy team will not be in the room with you during treatment. But they can see, hear and talk to you if you need them at any time. They will tell you what to expect and how many sessions of treatment you will have.
You can usually go home after SRT. You will not be radioactive and it is safe for you to be with other people.
Side effects will depend on your exact treatment. Your doctor will tell you what is likely in your situation. They may give you steroids to prevent side effects. Tell them if you have any side effects so they can help.
Some of these are a newer treatments that may not be available in all hospitals which decreases side effects and allows better control and treatment of the tumor.
Chemoradiation
Sometimes chemotherapy is given at the same time as radiotherapy. This is called chemoradiation or chemoradiotherapy. Chemotherapy uses anti-cancer (cytotoxic) drugs to destroy cancer cells. The chemotherapy drugs can make cancer cells more sensitive to radiotherapy. This can help radiotherapy to work better. This is only helpful for certain types of cancer, so it is not suitable for everyone.
External beam radiotherapy is given from a radiotherapy machine outside the body. The radiotherapy machine does not usually touch you. Treatment usually only takes a few minutes and is not painful.
This treatment is normally given as a number of short, daily treatments in a radiotherapy department. These are called treatment sessions or fractions. It is given using a machine that looks like a large x-ray machine or CT scanner.
You usually have external beam radiotherapy as an outpatient. The number of treatment sessions you have will depend on the type of cancer you have and the aim of the treatment. The doctor will explain the treatment plan to you.
Before Treatment
Radiotherapy is carefully planned for each person by a team of the experts radiation oncologists, a medical physician, and a radiation physicist.
Your radiotherapy team will explain what to expect. Your first planning visit usually takes between 30 to 60 minutes. You will have scans of the area to be treated. This helps the radiotherapy team decide the exact dose of radiotherapy and what area to treat.
During planning, the radiotherapy staff may make a small permanent mark (like a tattoo) on your skin. This is to show the exact place the radiotherapy should be given
You may need a mould or mask for your radiotherapy. These help you stay still in the correct position. Molds are for a leg, arm, or another body part. You only need a mask if you are having radiotherapy to your head or neck. It fits tightly but it should not be uncomfortable. You only wear it for during your planning and while you are having the radiotherapy.
Before you start your treatment, it needs to be planned. This is to make sure that the radiotherapy is aimed precisely at cancer. This will also mean it causes the least possible damage to the surrounding tissue. Your radiotherapy team will plan your radiotherapy carefully.
Our team uses all diagnostic imaging (PET-CT, MRI, CT) to define treatment volumes and organs at risk. This makes it very accurate for treatment planning. Our team uses the latest recommendations (European and American) to give the most appropriate treatment for our patients.
Treatment sessions
Usually, each radiotherapy appointment takes about 10 to 20 minutes. The treatment itself usually only takes a few minutes < 5 minutes. Most of the appointment is spent getting you into the correct position and checking your details.
Before your first treatment, the medical team explains what you will see and hear. It is normal to feel a bit nervous about having your treatment. But, as you get to know the staff and understand what to expect, it usually gets easier. You can talk to the staff about any worries you have.
Positioning you for treatment
Before your treatment, the radiation physicist may ask you to change into a hospital dress. This is so they can easily reach the marks on your skin that show the treatment area.
The radiation physicist helps you onto the treatment couch and position you carefully. They also adjust the height and position of the couch. They will talk you through what they are doing.
The radiation physicist looks at the marks on your skin (or on your mask or mold, if you have one). This is to help get you in the same position you were in for your planning scan. They help you arrange your clothes so that the area of your body being treated is bare. They are careful to protect your privacy so that nobody else can see you.
It is important that you are comfortable, as you have to lie as still as possible during the treatment. The room may be quite dark to help the radiation physicist while they are getting you into the correct position.
Your radiation physicist will tell you how long your treatment will take. When you are in the correct position, they leave the room, and you are given your treatment. There is a camera, so they can see you from outside the room. There is usually an intercom, so you can talk to them if you need to during your treatment.
During treatment
The radiotherapy machine does not usually touch you.
The treatment itself is painless. You may hear a slight buzzing noise from the radiotherapy machine while you are having the treatment.
Some treatment rooms have music players, so you can listen to music to help you relax. If you would like to listen to your own music, ask us.
The radiation physicist may take pictures (x-rays or CT scans) of the treatment area during your treatment. They may be taken on the first day and again on other days. These pictures are used to help make sure the treatment is given accurately. They are not used to show how well treatment is working, as the treatment takes time to work.
Once your treatment session has finished, the radiation physicist will come and help you off the treatment couch. It is important to wait until they tell you it is ok to move. Then you can get ready to go home, or back to the ward if you are having treatment as an inpatient.
External beam radiotherapy does not make you radioactive. It is safe for you to be with other people, including children, throughout your treatment. It is also safe to have sex.
Our medical team treats cancer patients every day. Our goal is to adopt the most optimal treatment to each patient. We treat by respecting the latest international guidelines and advanced research. The different devices available are radiotherapy, immunotherapy, targeted therapies, chemotherapy, and anti-hormonal treatment. We can use a combination of several treatments.
We work with international experts to ensure that our patients are treated as best as possible with the latest advances in research.
Immunotherapy also called biologic therapy, is a type of cancer treatment that boosts the body's natural defenses to fight cancer. It uses substances made by the body to improve or restore immune system function.
Targeted therapy works by targeting cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. These genes and proteins are found in cancer cells or in cells related to cancer growth, like blood vessel cells.
Radiotherapy technology in the Center of high Energy of Nice
Deliver the right dose of energy in the right place to kill cancer cells or prevent a recurrence.
It is a locoregional treatment that delivers energy (photons of 6 or 18 MegaVolt or electrons) in a target volume.
Its ambition is either curative, participate in the cure of cancer, or symptomatic, relieve or prevent the effects.
Radiation therapy by volume arc therapy with intensity modulation (VMAT), image-guided radiotherapy (onboard scanner), adaptive radiotherapy, and stereotactic radiotherapy (VERSA HD, Elekta) allow highly precise treatment. Radiation therapy is tailor-made. We have the last technology and linear accelerator.
All our radiotherapy is prepared And carried out at the Center of High Energy of Nice by our team of 4 medical physicists. graduated from France.
Radiation therapy is based on the use of ionizing radiation for therapeutic purposes and breaks the DNA of tumors cell. The one we deliver is also called external radiotherapy (the source is external to the body of the patient).
We have a high-tech technical platform with 3D radiotherapy and intensity modulation Arc-therapy:
• 1 synergy Elekta and 1 VERSA HD Elekta, with On-Board Imaging (OBI) and Image-Guided Radiotherapy (IGRT) technologies. • 1 virtual simulation computerized tomography/scanner dedicated to tracking and dosimetry
To prepare the treatment and be more accurate the medical and physicians teams practice a fusion of PET-CT images, CT images before surgery, and MRI images, with our CT images.
This allows us to delimit in a precise way the target volumes to be treated
- 1 Computerized Treatment Planning Systems (Velocity / Mosaiq / Monaco Elekta) : dosimetry network in three-dimensional, conformational radiotherapy, with intensity modulation.
- 1 system for checking and verifying treatment parameters (phantom Delta 4)
- 1 complete and modern set of device control tools.
- networked organization of medical and technical records, settings and images ensuring maximum security with the recording of all data.
External beam therapy with intensity modulation: volumetric arc therapy
All our radiotherapy is done in three-dimensional mode with intensity modulation (forward planning or, almost always for pelvic, abdominal, thoracic or brain by volume arc-therapy with intensity modulation
Stereotactic radiotherapy
The Center of high energy has a system dedicated to stereotactic radiotherapy with the VERSA HD. Our latest generation of linear accelerator performs images before the treatment to detect if the patient and tumor is in the same position as the simulation scanner and corrects before the treatment to ensure its precision. The use of VERSA HD does not require any invasive compression system and allows the administration of very high doses, "ablative metastases or tumors", in a short session (1 to 6).
Dr and Pr René-Jean BENSADOUN,
Radiation Oncologist, Medical Dosctor, Physician Doctor (MD, PhD)
Professor in Radiation Oncology and Chairman, Centre de Haute Energie, NICE (France)
Fields of Interest: Radiation Oncology, Head & Neck Cancer, Supportive Care in Cancer, Low Level LaserTherapy, New techniques in Radiation Oncology (Intensity-Modulated Radiation Therapy), Cancer-treatment toxicity.
MAJOR of the first in Nice (June 1979)
Doctorate in Medicine (Nice, Oct. 1989).
Diploma of Specialized Studies (DES) of Oncology, Oncology Radiotherapy Oct. 1989
Diploma of Advanced Studies (DEA) in Radiobiology and Radiopathology (Sept. 1990).
Specialist Doctor of Centers for the Fight Against Cancer (CLCC) on Contest dated 23/10/91. Taking office from 01/11/91 at the Antoine-Lacassagne Center in Nice, Radiotherapy department.
Head of the East Radiotherapy Unit (Department of Radiotherapy) at Center of Antoine Lacassagne from 12/12/96 to 31/08/08 and Coordinator of the Department of Radiotherapy at Center of Antoine Lacassagne, in Nice from March 2007 to August 2008.
2008-2013: Head of Department, Radiation Oncology Department, Regional Cancer Center, University Hospital of Poitiers; Professor of Universities at the Faculty of Medicine and Pharmacy of Poitiers
145 Scientific Publications : https://www.ncbi.nlm.nih.gov/pubmed/?term=bensadoun+rj
Boards: President of the World Association for photobiomoduLation Therapy (2018), past-Vice-President (2017), past-Scientific Secretary (2015-2017) Member of Head & Neck Cancer French Groups Deputy Associate Editor of JSCC (Journal of Supportive Care in Cancer) Member of MASCC-ISOO Mucositis Board and Oral Care Board Member of ESMO Toxicity Working Group.
Dr. Idriss TROUSSIER, Medical Doctor
French nationality
Professional career
2013-today Medical Doctor, a specialist in radiation oncologist, medical oncologist
2018-today Medical Doctor of the university hospital of Geneva
2015 –2017 Medical Doctor of university hospital Pitié-Salpêtrière Paris hospital
2011 – 2017 Teacher and tutor for medical students to prepare medical exams
2010 – 2015 Residency of radiation oncology and medical oncology in the university hospital of Poitiers, Lausanne,
2003 – 2010 Medical student of University of Paris 5, first year rank 17th/2500
Diplomas
2013 Swiss and French medical diploma in radiation oncology
11/2016 French medical diploma in medical oncology
11/2017 University diploma, Paris 6, medical treatment of cancer
11/2016 University diploma, Paris 6, stereotactic radiotherapy
09/2015 University diploma Gustave Roussy in head and neck cancers
09/2014 University diploma Nice, in high technicity radiotherapy, streotactic technics, Volumetric arc therapy, cyber-knife
12/2013 Specialist Thesis of medical doctor in radiation oncology
2012 – 2013 Master of science : cancer genesis, pharmacology anti-cancer
Award & Publications
- « AWARD LUCIEN MALLET », award of the French Society of radiation oncology, radio-physics 2014: radiotherapy new techniques (modulated volume arc-therapy), advantages, disadvantages, clinical impact for digestive cancer
- Oral communication award of the French Society of cancerology Monaco Congress 2014 in head and neck cancer
Scientific Publications:
- Advances in the management of cervical lymphadenopathies of unknown primary with intensity modulated radiotherapy: Doses and target volumes. Cancer Radiother. 2018 May 3. pii: S1278-3218(18)30051-9. doi: 10.1016/j.canrad.2017.10.008.
- Advances in the management of cervical lymphadenopathies of unknown primary: advances in diagnostic imaging and surgical modalities and new international staging system. Bull Cancer. 2018 Feb;105(2):181-192. doi: 10.1016/j.bulcan.2017.11.009. Epub 2017 Dec 21.
- Quality and safety policy implementation for a new radiotherapy device. submitted to cancer radiotherapy 2018
- From bunker construction to patient treatment: quality controls applied to modern radiotherapy techniques submitted to cancer radiotherapy 2018
- Management of locally advanced anal canal carcinoma with intensity modulated radiotherapy and concurrent chemotherapy: a critical review of the literature, being submitted to critical review of oncology
- Chemoradiation for esophageal cancer : a critical review of the literature submitted to cancer radiotherapy 2018
- GORTEC clinical practice guidelines for the delineation of nodal target volumes in intensity modulated radiation therapy for head and neck cancers in submission in radiation oncology
- [Clinical research for rectal carcinoma: State of the art and objectives]. Cancer Radiother. 2017 Sep 7. pii: S1278-3218(17)30202-0. doi: 10.1016/j.canrad.2017.07.019. [Epub ahead of print] French.
- [Lung dose constraints for normo-fractionated radiotherapy and for stereotactic body radiation therapy]. Cancer Radiother. 2017 Sep 5. pii: S1278-3218(17)30344-X. doi: 10.1016/j.canrad.2017.07.046. [Epub ahead of print] French.
- Low level Laser therapy : a corner stone in the management of cancer therapy-Induced mucsitis Chapter 41 Handbook of low-level Laser therapy, 2017 Pan Stanford Publishing
- Adaptive radiation therapy in head and neck cancer for clinical practice: state of the art and practical challenges. Jpn J Radiol. 2017 Feb;35(2):43-52. doi: 10.1007/s11604-016-0604-9.
- Role of irradiation for patients over 80 years old with glioblastoma: a retrospective cohort study. J Neurooncol. 2016 Sep;129(2):347-53. doi: 10.1007/s11060-016-2182-1. Epub 2016 Jun 16.
- Efficacy and safety of helical tomotherapy with daily image guidance in anal canal cancer patients. Acta Oncol. 2016 Jun;55(6):767-73. doi: 10.3109/0284186X.2015.1120886. Epub 2016 Apr 1.
- [Clinical and paraclinical follow-up after radiotherapy for head and neck cancer]. Cancer Radiother. 2015 Oct;19(6-7):597-602. doi: 10.1016/j.canrad.2015.05.017. Epub 2015 Aug 13. French.
- [Mucosal melanomas of the head and neck: State of the art and current controversies]. Bull Cancer. 2015 Jun;102(6):559-67. doi: 10.1016/j.bulcan.2015.04.013. Epub 2015 May 26. French.
- [Management of locally advanced anal canal carcinoma with modulated arctherapy and concurrent chemotherapy].Cancer Radiother. 2015 Apr;19(2):127-38. doi: 10.1016/j.canrad.2014.12.005. Epub 2015 Mar 12. French.
- [Lymph node metastases from squamous cell carcinoma of unknown primary site. Is it time to change of paradigm?]. Hamoir M, Troussier I, Machiels JP, Reychler H, Schmitz S, Thariat J, Grégoire V. Bull Cancer. 2014 May 1;101(5):455-60. doi: 10.1684/bdc.2014.1965. Review. French.
- Cervical node of unknown primary: patterns of care and factors influencing the choice of clinical target volumes. Oral Oncol. 2014 May;50(5):e25-6.
- [Target volumes in cervical lympadenopathies of unknown primary: toward a selective customized approach? On behalf of REFCOR]. Cancer Radiother. 2013 Nov;17(7):686-94. doi: 10.1016/j.canrad.2013.07.132. Epub 2013 Oct 4. Review. French.
Scientific Posters / oral communication congress :
- Uni or bilateral irradiation in cervical lymph node metastases of unknown primary? Electronic Poster : MO_41_2858, ASTRO 2018
- Should neoadjuvant chemo-radiotherapy for esophageal cancers be adapted to histology? Literature Data Analysis, Poster SFRO 2018
- Chemo-radiotherapy of pancreatic cancers: why and how to protect the spleen. Poster SFRO, octobre 2018
- Uni. or bilateral irradiation of cervical lymph node metastases of unknown primary ?
Oral Communication Submission, SFRO, octobre 2018
- Immune checkpoint inhibitors and sereotactic radiosurgery (SRS) in melanoma brain metastases. ASCO online publication 2018, abstract 225009
- Proposition of splenic dose-volume constraints to prevent severe lymphopenia after chemoradiation for pancreatic cancer. Astro 2018
- Indications for external beam radiotherapy in differentiated thyroid carcinoma: an expert consensus – ESTRO 2018
- Contemporary esophageal cancer management by chemo radiation: survey of French radiation oncologists – ESTRO 2018
- Whole brain radiotherapy and concurrent temozolomide in multifocal and/or multicentric newly diagnosed glioblastoma – ESTRO 2018
- 894P - A retrospective study of the management of metastatic renal cell carcinoma brain tumors Annals of Oncology (2017) 28 (suppl_5): v295-v329. 10.1093/annonc/mdx371
- Comparison of clinical target volumes between Phase III trials of exclusive chemoradiotherapy for esophageal cancers Cancer/Radiothérapie, Volume 21, Issues 6–7, Poster October 2017, Pages 695-696,
- Management of patients with esophageal cancer by chemoradiotherapy: national multicentre practice survey, Cancer/Radiotherapy, Volume 21, Issues 6, 7 Poster SFRO October 2017, Page 681
- Mono-isocentric conformational art therapy for multiple brain metastases: automated planning and dosimetric comparison with Gammaknife® Perfexion™ Volume 21, Issues 6–7, Poster SFRO October 2017, Pages 685-686
- Role of the manipulator in medical quality electroradiology in the implementation of modulated volumetric arcthérapie in a radiotherapy department, Cancer/Radiothérapie, Volume 19, Issues 6–7, Poster SFRO, October 2015, Pages 694
- Focal dose escalation on the tumor index by associated high dose rate brachytherapy and three-dimensional conformational radiotherapy. Cancer/Radiothérapie, Volume 19, Issues 6–7, Poster SFRO, October 2015, Pages 671-672
- Localized, intermediate or high-risk prostate cancer whose treatment was external radiation therapy and included high dose rate brachytherapy: Cancer/Radiothérapie, Volume 18, Issues 5–6, Poster SFRO October 2014, Page 622


















